Connect With Us
vendor
Risk Factors and Treatment of Bunions
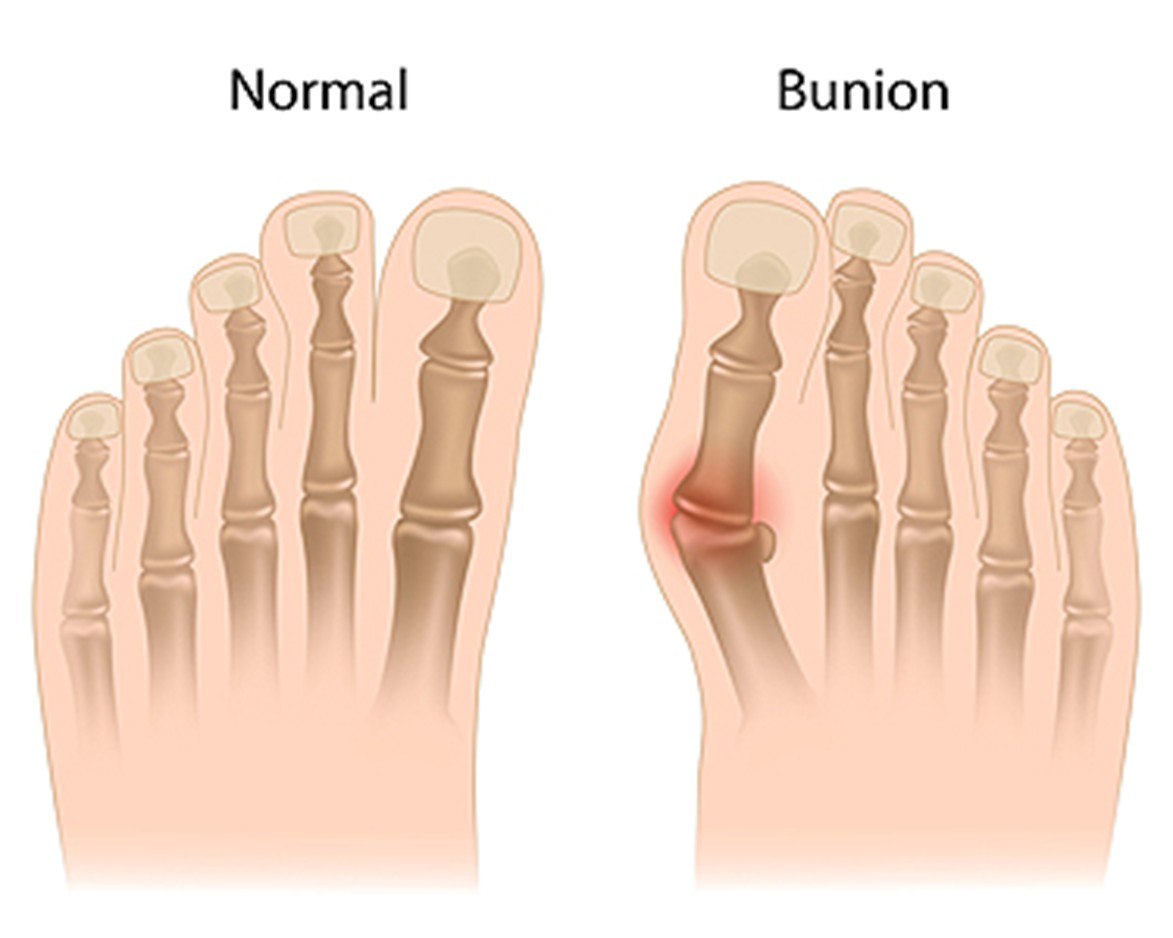 A bunion is a deformity of the joint at the base of the big toe, where the bones gradually shift out of alignment. This happens when the tip of the big toe leans toward the smaller toes, forcing the metatarsal bone inward and forming a bony lump at the joint. Bunions may develop slowly over years, or appear more rapidly in adolescents. Risk factors include family history, wearing shoes that squeeze the toes, inflammatory joint diseases like rheumatoid arthritis, and structural foot problems, such as over-pronation. Bunions often cause pain, redness, swelling, and thickened skin over the joint. A podiatrist can help by providing supportive devices to ease pressure and correcting foot mechanics. In severe cases, surgery may be required to realign the bones and relieve pain. If you have a bunion that is interfering with your daily activities, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment options.
A bunion is a deformity of the joint at the base of the big toe, where the bones gradually shift out of alignment. This happens when the tip of the big toe leans toward the smaller toes, forcing the metatarsal bone inward and forming a bony lump at the joint. Bunions may develop slowly over years, or appear more rapidly in adolescents. Risk factors include family history, wearing shoes that squeeze the toes, inflammatory joint diseases like rheumatoid arthritis, and structural foot problems, such as over-pronation. Bunions often cause pain, redness, swelling, and thickened skin over the joint. A podiatrist can help by providing supportive devices to ease pressure and correcting foot mechanics. In severe cases, surgery may be required to realign the bones and relieve pain. If you have a bunion that is interfering with your daily activities, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment options.
If you are suffering from bunions, contact one of our clinicians from The Footcare Centre. Our podiatrists can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of bony growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
How a Podiatrist Can Help People With Flat Feet
 Flat feet, also known as fallen arches, occur when the arches of the feet collapse, causing the entire sole to touch the ground. This condition can be present from birth or develop over time due to injury, aging, obesity, or certain medical conditions. Symptoms include foot pain, swelling, fatigue, or difficulty standing or walking for long periods. Some people experience knee or back discomfort as well. Relief often comes from wearing supportive shoes, custom orthotics, or stretching exercises. A podiatrist can evaluate the structure of your feet, identify the underlying cause, and recommend a personalized treatment plan. If you have flat feet and have persistent foot pain, it is suggested that you consult a podiatrist for effective relief and improved foot function.
Flat feet, also known as fallen arches, occur when the arches of the feet collapse, causing the entire sole to touch the ground. This condition can be present from birth or develop over time due to injury, aging, obesity, or certain medical conditions. Symptoms include foot pain, swelling, fatigue, or difficulty standing or walking for long periods. Some people experience knee or back discomfort as well. Relief often comes from wearing supportive shoes, custom orthotics, or stretching exercises. A podiatrist can evaluate the structure of your feet, identify the underlying cause, and recommend a personalized treatment plan. If you have flat feet and have persistent foot pain, it is suggested that you consult a podiatrist for effective relief and improved foot function.
Flatfoot is a condition many people suffer from. If you have flat feet, contact of our clinicians from The Footcare Centre. Our podiatrists will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions, please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a condition that occurs when the arches on the foot are flattened, which allows the soles of the feet to touch the floor. Flatfoot is a common condition and it is usually painless.
Throughout childhood, most people begin to develop arches in their feet, however, some do not. Those who do not develop arches are left with flatfoot. The pain associated with flat feet is usually at its worse when engaging in activity. Another symptom that may occur with those who have this condition is swelling along the inside of the ankle.
It is also possible to have flexible flatfoot. Flexible flatfoot occurs when the arch is visible while sitting or standing on the tiptoes, but it disappears when standing. People who have flexible flatfoot are often children and most outgrow it without any problems.
There are some risk factors that may make you more likely to develop flatfoot. Those who have diabetes and rheumatoid arthritis have an increased risk of flatfoot development. Other factors include aging and obesity.
Diagnosis for flat feet is usually done by a series of tests by your podiatrist. Your podiatrist will typically try an x-ray, CT scan, ultrasound, or MRI on the feet. Treatment is usually not necessary for flat foot unless it causes pain. However, therapy is often used for those who experience pain in their flat feet. Some other suggested treatment options are arch supports, stretching exercises, and supportive shoes.
How to Treat and Prevent Foot Corns
 Foot corns are thick, hardened areas of skin that develop from pressure or friction, often caused by wearing tight shoes or abnormal foot structure. They commonly form on the tops and sides of toes or the soles of the feet. While they are not usually serious, corns can become painful if not treated. Treatment starts by reducing the pressure that caused the corn. Wearing properly fitting shoes with a wide toe box can help and prevent corns. Using protective pads or custom orthotics may relieve pressure and prevent corns from coming back. It is important not to trim or cut corns by yourself, especially if you have diabetes. If you have a painful foot corn, it is suggested that you see a podiatrist who can safely remove corns, and address any underlying issues causing them.
Foot corns are thick, hardened areas of skin that develop from pressure or friction, often caused by wearing tight shoes or abnormal foot structure. They commonly form on the tops and sides of toes or the soles of the feet. While they are not usually serious, corns can become painful if not treated. Treatment starts by reducing the pressure that caused the corn. Wearing properly fitting shoes with a wide toe box can help and prevent corns. Using protective pads or custom orthotics may relieve pressure and prevent corns from coming back. It is important not to trim or cut corns by yourself, especially if you have diabetes. If you have a painful foot corn, it is suggested that you see a podiatrist who can safely remove corns, and address any underlying issues causing them.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact of our clinicians from The Footcare Centre. Our podiatrists will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions, please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Types of Surgery for Hammertoes
 Hammertoes, a deformity where the toe bends upward at the middle toe joint, can cause significant discomfort. When conservative treatments fail, surgery may provide lasting relief. Several surgical options are based on the flexibility of the affected joint, often in the second toe. Tendon transfer surgery is often used for a flexible hammertoe, where tendons are repositioned to straighten the toe and restore balance. For rigid hammertoes, surgery involves cutting tendons and ligaments, sometimes removing part of the bone, and stabilizing the toe with temporary pins. Fusion surgery may also be performed, which removes parts of the joint to allow bones to fuse together, resulting in a straighter, more stable toe. In severe cases, amputation may be considered, but this is rare and typically reserved for extreme pain when no other treatments work. A podiatrist can assess the type and severity of a hammertoe to determine the most appropriate surgical approach to relieve pain and restore foot function. If you are experiencing pain from a hammertoe, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Hammertoes, a deformity where the toe bends upward at the middle toe joint, can cause significant discomfort. When conservative treatments fail, surgery may provide lasting relief. Several surgical options are based on the flexibility of the affected joint, often in the second toe. Tendon transfer surgery is often used for a flexible hammertoe, where tendons are repositioned to straighten the toe and restore balance. For rigid hammertoes, surgery involves cutting tendons and ligaments, sometimes removing part of the bone, and stabilizing the toe with temporary pins. Fusion surgery may also be performed, which removes parts of the joint to allow bones to fuse together, resulting in a straighter, more stable toe. In severe cases, amputation may be considered, but this is rare and typically reserved for extreme pain when no other treatments work. A podiatrist can assess the type and severity of a hammertoe to determine the most appropriate surgical approach to relieve pain and restore foot function. If you are experiencing pain from a hammertoe, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact one of our clinicians from The Footcare Centre. Our podiatrists will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions, please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions from your podiatrist is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Finding Relief From Heel Pain
 Heel pain can interfere with your ability to walk comfortably and stay active. It often develops from overuse, wearing poor footwear, or an underlying condition such as plantar fasciitis. The discomfort may appear gradually or suddenly, especially after periods of rest. Choosing supportive shoes with proper cushioning can reduce strain on the heel. Stretching exercises for the calf muscles and the bottom of the foot may also help improve flexibility and ease tension. Resting the foot is a common first step when pain appears. In some cases, custom orthotics or other conservative treatments may be necessary to address the root cause. Persistent or worsening heel pain should not be ignored, as it can affect your balance and overall mobility. If heel pain is interfering with your daily activities, it is suggested that you see a podiatrist for a diagnosis and appropriate treatment.
Heel pain can interfere with your ability to walk comfortably and stay active. It often develops from overuse, wearing poor footwear, or an underlying condition such as plantar fasciitis. The discomfort may appear gradually or suddenly, especially after periods of rest. Choosing supportive shoes with proper cushioning can reduce strain on the heel. Stretching exercises for the calf muscles and the bottom of the foot may also help improve flexibility and ease tension. Resting the foot is a common first step when pain appears. In some cases, custom orthotics or other conservative treatments may be necessary to address the root cause. Persistent or worsening heel pain should not be ignored, as it can affect your balance and overall mobility. If heel pain is interfering with your daily activities, it is suggested that you see a podiatrist for a diagnosis and appropriate treatment.
Many people suffer from bouts of heel pain. For more information, contact one of our clinicians from The Footcare Centre. Our podiatrists can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions, please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
