Connect With Us
vendor
Different Types of Open Foot Wounds
 Open wounds on the feet are injuries that break the skin's surface, leaving underlying tissue exposed. Each type of open wound has distinct signs and characteristics. Abrasions, commonly referred to as scrapes, occur when skin on the foot experiences superficial damage from rubbing against a rough surface. Lacerations are cuts caused by sharp objects, which may vary in depth and severity depending on the force of the injury. Puncture wounds in the foot occur when a sharp object penetrates the skin, creating a small hole that can lead to deep tissue damage and infection if not properly treated. Avulsions, which often result from traumatic injuries in feet, involve the tearing away of skin and tissue from the body. Surgical wounds are intentional incisions made during surgical procedures. These open-foot wounds require careful monitoring and care to prevent complications during and after the procedure. Diabetic ulcers are open wounds often found on the feet of diabetics, resulting from poor circulation and nerve damage. Regardless of the type, appropriate wound care can decrease risk of infection in the foot and promote healing. If you're experiencing challenges with open wounds, it's suggested to consult with a podiatrist for effective treatment and management, reducing complications and supporting a successful recovery.
Open wounds on the feet are injuries that break the skin's surface, leaving underlying tissue exposed. Each type of open wound has distinct signs and characteristics. Abrasions, commonly referred to as scrapes, occur when skin on the foot experiences superficial damage from rubbing against a rough surface. Lacerations are cuts caused by sharp objects, which may vary in depth and severity depending on the force of the injury. Puncture wounds in the foot occur when a sharp object penetrates the skin, creating a small hole that can lead to deep tissue damage and infection if not properly treated. Avulsions, which often result from traumatic injuries in feet, involve the tearing away of skin and tissue from the body. Surgical wounds are intentional incisions made during surgical procedures. These open-foot wounds require careful monitoring and care to prevent complications during and after the procedure. Diabetic ulcers are open wounds often found on the feet of diabetics, resulting from poor circulation and nerve damage. Regardless of the type, appropriate wound care can decrease risk of infection in the foot and promote healing. If you're experiencing challenges with open wounds, it's suggested to consult with a podiatrist for effective treatment and management, reducing complications and supporting a successful recovery.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our clinicians from The Footcare Centre. Our podiatrists will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a podiatrist—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Nerve Pain in the Foot
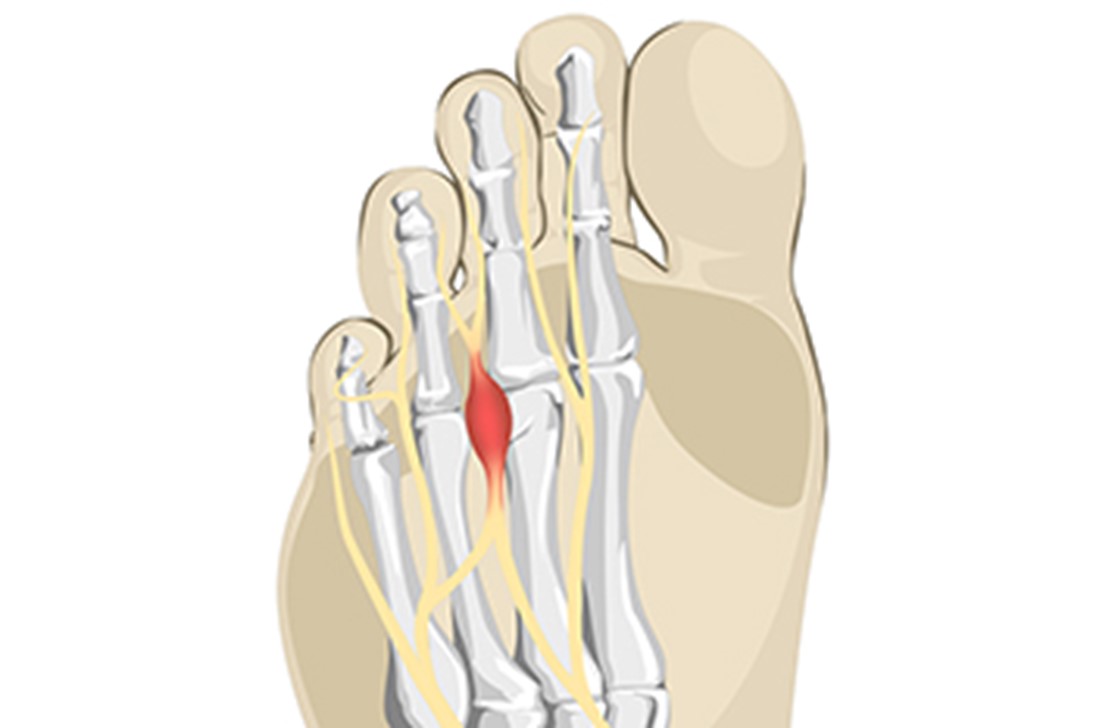 Experiencing nerve pain in your foot can impact your daily activities and overall quality of life. One common cause of such pain is Morton's neuroma, a condition where a nerve in the ball of the foot becomes swollen or thickened. This often results from wearing shoes that squeeze the toes together for extended periods, such as high-heeled, tight, or narrow footwear. Symptoms of Morton's neuroma can include a sharp, burning pain in the foot that intensifies with walking and a sensation of a small lump in the ball of the foot, typically between the third and fourth toes. Diagnosis usually involves a physical exam and may require imaging tests like ultrasound, X-ray, or MRI scans to confirm. Switching to shoes that allow ample room for the toes and reducing activities that exacerbate the pain may provide relief. If these measures are insufficient, special pads or devices to spread the toes, steroid injections, or in severe cases, surgery, may be recommended to alleviate symptoms. Persistent nerve pain should not be ignored, as early intervention can prevent further complications. If you are experiencing such pain, consulting a podiatrist is suggested for a comprehensive evaluation and appropriate treatment plan.
Experiencing nerve pain in your foot can impact your daily activities and overall quality of life. One common cause of such pain is Morton's neuroma, a condition where a nerve in the ball of the foot becomes swollen or thickened. This often results from wearing shoes that squeeze the toes together for extended periods, such as high-heeled, tight, or narrow footwear. Symptoms of Morton's neuroma can include a sharp, burning pain in the foot that intensifies with walking and a sensation of a small lump in the ball of the foot, typically between the third and fourth toes. Diagnosis usually involves a physical exam and may require imaging tests like ultrasound, X-ray, or MRI scans to confirm. Switching to shoes that allow ample room for the toes and reducing activities that exacerbate the pain may provide relief. If these measures are insufficient, special pads or devices to spread the toes, steroid injections, or in severe cases, surgery, may be recommended to alleviate symptoms. Persistent nerve pain should not be ignored, as early intervention can prevent further complications. If you are experiencing such pain, consulting a podiatrist is suggested for a comprehensive evaluation and appropriate treatment plan.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our clinicians from The Footcare Centre. Our podiatrists will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. They will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the podiatrist may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Effective Foot Stretches for Dancers and Ballet
 Foot stretches are vital for dancers and ballet enthusiasts to maintain flexibility and prevent injuries. The seated foot stretch, where you extend your leg and gently pull back on your toes, helps lengthen the arch and Achilles tendon. Performing ankle circles, both clockwise and counterclockwise, increases mobility and reduces stiffness. The towel stretch, where you use a towel around the ball of the foot and pull gently, provides a deep stretch to the sole and calf muscles. Additionally, stretching the toes by spreading and pressing them individually enhances dexterity and control. These stretches, when practiced regularly, improve foot flexibility, promote better alignment, and prepare the feet for the demands of dancing. Foot injuries can easily happen from practicing inadequate foot stretches. If this applies to you, it is suggested that you consult a podiatrist who can diagnose and treat foot pain.
Foot stretches are vital for dancers and ballet enthusiasts to maintain flexibility and prevent injuries. The seated foot stretch, where you extend your leg and gently pull back on your toes, helps lengthen the arch and Achilles tendon. Performing ankle circles, both clockwise and counterclockwise, increases mobility and reduces stiffness. The towel stretch, where you use a towel around the ball of the foot and pull gently, provides a deep stretch to the sole and calf muscles. Additionally, stretching the toes by spreading and pressing them individually enhances dexterity and control. These stretches, when practiced regularly, improve foot flexibility, promote better alignment, and prepare the feet for the demands of dancing. Foot injuries can easily happen from practicing inadequate foot stretches. If this applies to you, it is suggested that you consult a podiatrist who can diagnose and treat foot pain.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with one of our clinicians from The Footcare Centre. Our podiatrists will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Being the backbone of the body, the feet carry your entire weight and can easily become overexerted, causing cramps and pain. As with any body part, stretching your feet can serve many benefits. From increasing flexibility to even providing some pain relief, be sure to give your feet a stretch from time to time. This is especially important for athletes or anyone performing aerobic exercises, but anyone experiencing foot pain or is on their feet constantly should also engage in this practice.
Great ways to stretch your feet:
- Crossing one leg over the others and carefully pull your toes back. Do 10-20 repetitions and repeat the process for each foot
- Face a wall with your arms out and hands flat against the wall. Step back with one foot and keep it flat on the floor while moving the other leg forward. Lean towards the wall until you feel a stretch. Hold for 30 seconds and perform 10 repetitions for each foot
- Be sure not to overextend or push your limbs too hard or you could risk pulling or straining your muscle
Individuals who tend to their feet by regular stretching every day should be able to minimize foot pain and prevent new problems from arising.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stretching Your Feet
Debilitating foot pain is a problem for many people. But just as stretching the torso can help alleviate back pain, stretching the feet can also help mend existing foot problems and prevent future ones.
The feet, as the body’s foundation, carry the body’s entire weight and can get easily strained from overexertion. Persistent sharp pain and cramping in the feet are often common concerns. Foot pain and foot problems can be due to any number of causes, and in many cases pain may be eased without medication or doctor visits. It is always a good idea, however, to first rule out any serious medical issues with a podiatrist.
Stretching can help relax the feet and alleviate pain, but is especially important before heavy aerobic exercise. Stretching before such activities can help you avoid experiencing painful cramps or strained foot muscles. Stretches should be performed slowly and deliberately without forceful pulling. The stretch should be held for several seconds before relaxing.
A great way to stretch out and loosen up the foot muscles while sitting is to cross one leg over the other and pull the toes carefully back without overextending. Start by resting the left ankle on the right knee. With the left hand, gently flex the left foot by pulling back on the toes. Do not pull too hard; just hard enough to feel the stretch in the arch of the foot. Then point the toes of the left foot as far as you can. Rotate the motion of pointing with pulling back on the toes. This should relax and stretch the muscles on the bottom and the top of the foot. Doing this stretch ten to twenty times should bring relief. Repeat the whole process for the other foot by resting the right ankle on the left knee.
A stretch that focuses on the often injured Achilles tendon involves standing and facing a wall with your arms out and hands flat against the wall. Step back with one foot, keeping it flat against the floor. Move the other leg forward and lean toward the wall. You should feel a stretch through the back of your leg and your Achilles tendon, but do not push yourself too much. Stop when you feel a stretching sensation, and hold for 30 seconds. Ten repetitions may be done for each foot.
Stretching the feet is important for athletes or those performing aerobic exercise, but it can also help anyone with foot pain caused by poor footwear, plantar fasciitis, or long hours standing and walking. Individuals who tend to their feet by regularly stretching every day should be able to minimize foot pain and prevent new problems from arising.
Women’s Foot Health
 As women enter their 40s, specific foot care becomes important to maintain overall health and mobility. Common foot issues like plantar fasciitis, bunions, and arthritis can affect women more significantly due to factors like hormonal changes, pregnancy, and footwear choices over the years. To avoid exacerbating these issues, it is beneficial for women to steer clear of high heels and narrow-toed shoes, which can lead to foot deformities and chronic pain. Additionally, prolonged wearing of flip-flops or flats without proper support can strain the arches and contribute to plantar fasciitis. Instead, opt for supportive footwear with cushioning and roomy toe boxes to accommodate natural foot shape and reduce pressure points. Regular foot exercises and stretches can also help alleviate discomfort and maintain flexibility. If you are a female and experiencing problems with your feet as you age, it is suggested that you consult a podiatrist for personalized care and treatment for long-term foot health.
As women enter their 40s, specific foot care becomes important to maintain overall health and mobility. Common foot issues like plantar fasciitis, bunions, and arthritis can affect women more significantly due to factors like hormonal changes, pregnancy, and footwear choices over the years. To avoid exacerbating these issues, it is beneficial for women to steer clear of high heels and narrow-toed shoes, which can lead to foot deformities and chronic pain. Additionally, prolonged wearing of flip-flops or flats without proper support can strain the arches and contribute to plantar fasciitis. Instead, opt for supportive footwear with cushioning and roomy toe boxes to accommodate natural foot shape and reduce pressure points. Regular foot exercises and stretches can also help alleviate discomfort and maintain flexibility. If you are a female and experiencing problems with your feet as you age, it is suggested that you consult a podiatrist for personalized care and treatment for long-term foot health.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our clinicians from The Footcare Centre. Our podiatrists will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your podiatrist to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Dealing With Achilles Tendon Ruptures
 Diagnosing Achilles tendon ruptures involves a combination of clinical evaluation and imaging tests. The Achilles tendon, the largest tendon in the body, connects the calf muscles to the heel bone. A rupture occurs when this tendon tears, often due to sudden or forceful movements during sports or activities that place excessive stress on the tendon. Symptoms of an Achilles tendon rupture typically include a sudden, sharp pain in the back of the ankle or calf, accompanied by swelling and difficulty walking or standing on tiptoe. While this injury can happen to anyone, factors such as age, sports participation, and pre-existing foot problems like flat feet or tendonitis may increase the risk. Treatment options include conservative measures like immobilization to more advanced options, like surgical repair for severe cases. If you have injured your Achilles tendon, it is strongly suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and treatment plan.
Diagnosing Achilles tendon ruptures involves a combination of clinical evaluation and imaging tests. The Achilles tendon, the largest tendon in the body, connects the calf muscles to the heel bone. A rupture occurs when this tendon tears, often due to sudden or forceful movements during sports or activities that place excessive stress on the tendon. Symptoms of an Achilles tendon rupture typically include a sudden, sharp pain in the back of the ankle or calf, accompanied by swelling and difficulty walking or standing on tiptoe. While this injury can happen to anyone, factors such as age, sports participation, and pre-existing foot problems like flat feet or tendonitis may increase the risk. Treatment options include conservative measures like immobilization to more advanced options, like surgical repair for severe cases. If you have injured your Achilles tendon, it is strongly suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and treatment plan.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our clinicians from The Footcare Centre. Our podiatrists can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a healthcare profressional.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Weybridge, UK. We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
